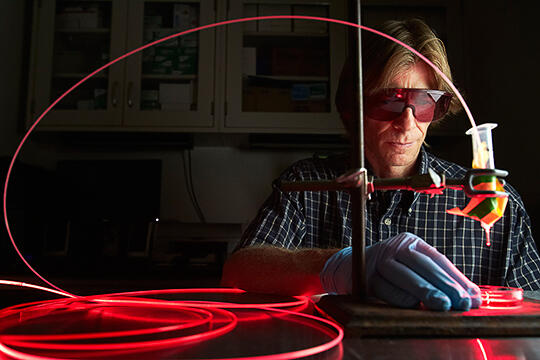
School of Allied Health Sciences' Steen Madsen is exploring new treatment methods for primary brain tumors -- tumors that originate in the brain -- using nanoparticles and lasers.
Madsen, professor and chair for the department of health physics and diagnostic sciences, is collaborating with Henry Hirschberg, a researcher at the University of California-Irvine's Beckman Laser Institute and Medical Clinic, on a particularly promising approach. It involves using a type of white blood cell that ingests foreign material as a therapeutic-drug delivery vehicle.
There are approximately 34,000 new cases of primary brain tumors diagnosed each year in the U.S. and Europe. Close to 40 percent of these tumors are of the most aggressively malignant variety, glioblastoma multiforme (GBM). Less than 5 percent of patients diagnosed with GBM will live more than five years.
Glioblastoma tumors are notoriously aggressive and difficult to treat. When removed during surgery, they almost always reappear. Madsen, Hirschberg, and their research team are exploring a small solution to this big problem: employing macrophages, the aforementioned, material-ingesting white blood cells, to transport nano-sized particles of therapeutic gold to surgical resection sites. If successful, it's a system that could greatly enhance the effectiveness of photothermal therapy, a process that destroys tumor cells using laser light.
Why gold? The precious metal offers two particular advantages. First, it has already been used safely in humans for a variety of medical applications. Second, and more to the point, gold has the ability to convert infrared laser energy to thermal energy. When exposed to photothermal therapy, gold nanoparticles act as heat generators and burn the tumor cells.
In preliminary studies, Madsen and Hirschberg demonstrated the feasibility of using macrophages as delivery vehicles for gold-based nanoparticles. This was a particularly welcome finding given that, being part of the body's natural defenses, macrophages can be easily extracted from a patient, loaded with the desired therapeutic agents and re-injected into the body.
During the study's next phase, Madsen and Hirschberg's team showed that using gold-loaded macrophages in concert with photothermal therapy was effective in treating tumor cells in the brains of laboratory animals. Animals that received the macrophages and photothermal therapy, in fact, showed zero tumor cells when the treatments concluded. These findings and others have been published in the Annals of Biomedical Engineering and Lasers in Surgery and Medicine.
Hurdles remain, however. Part of Madsen and Hirschberg's current research involves searching for a means to allow nanoparticle-loaded macrophages to pass through the body's "blood-brain barrier," the biological mechanism preventing most external cells and other matter from passing through to the brain. Thus far, the answer has eluded them.
Madsen and Hirschberg say they are confident that this obstacle, too, can be overcome, and that, once bypassed, they will be that much closer to improving the dismal five-year survival rate of GBM patients.