One of the first things to think about in the journey of becoming a doctor is education. How does someone train to become a doctor? What goes into this training?
Before applying to medical school, applicants must complete the prerequisites for medical school and obtain a bachelor’s degree. Once accepted into a medical school, training to become a doctor is split into two parts:
- Undergraduate medical education – when future physicians learn the foundations of medicine, gain clinical skills, and obtain their doctor of medicine degree once completed
- Graduate medical education – when they get to further enhance their clinical skills, work in their desired specialties, and become fully licensed.
Doctor of Medicine Degree Program
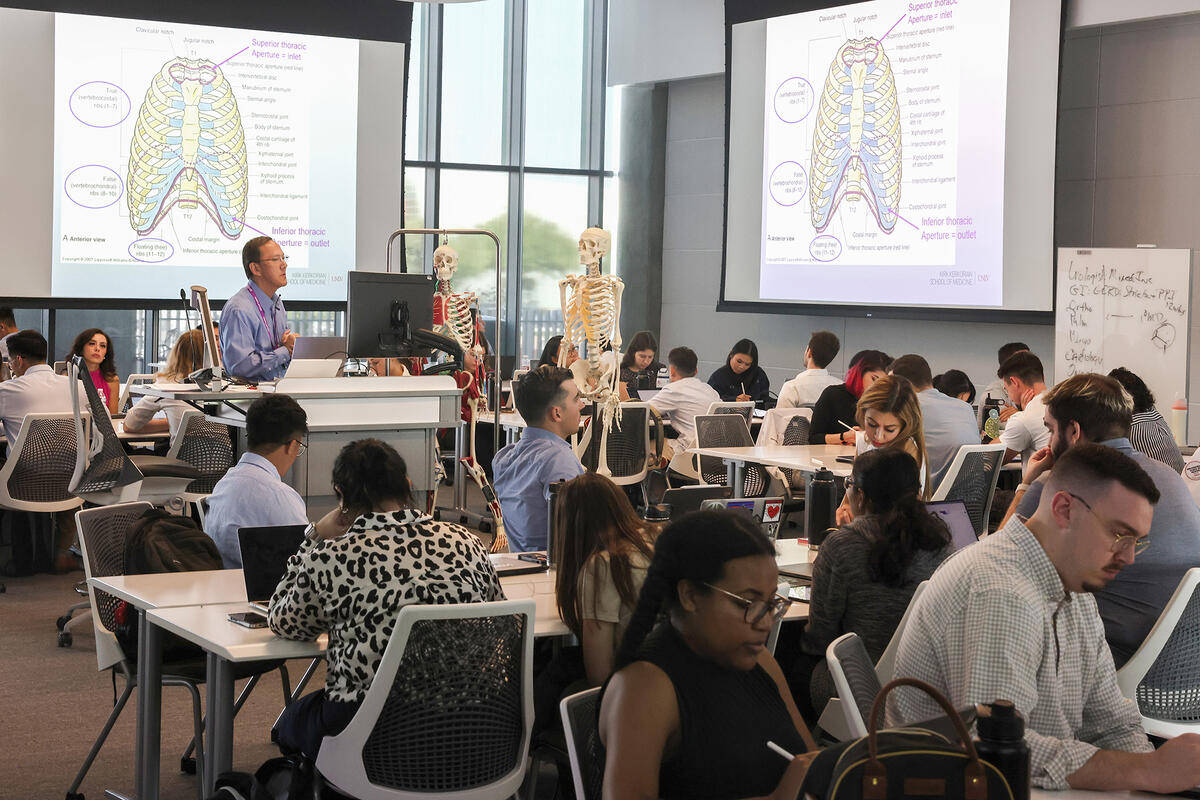
The Kirk Kerkorian School of Medicine at UNLV’s undergraduate medical education consists of a four-year doctor of medicine (MD) program that is split into three phases of study: foundations, clerkships, and career exploration.
Corrin Sullivan, assistant dean for curriculum, says, “In undergraduate medical education, our primary purpose is really to introduce students to the underlying foundations of medical science and its application in patient cases.”
The first phase, foundations, provides an introduction to medical science and also includes hands-on experience with standardized patients in the school’s foundations of clinical practice courses. Through these longitudinal series of classes, medical students are able to work with standardized patients — a.k.a. patient actors — under the supervision and guidance of MD faculty and doctor mentors. Students learn how to ask patients questions, do thorough histories and physical examinations, and apply clinical reasoning to identify the signs and symptoms presented in order to properly document a patient’s medical and personal history to help diagnosis, assessment, and management of their health.
This first phase is 18 months long and then students move on to the second phase of the program: clerkships.
Dr. Sullivan notes that this is a bit accelerated when compared to other medical schools, but because the students get so much “hands-on skills practice and simulation within those first 18 months,” they are able to get a six-month head start into their clinical studies, where they are able to utilize the skills they acquired from the foundations phase and gain practical, real-life learning experiences in a clinical setting.
During their clerkships, students have to complete rotations in the six core specialties – family medicine, internal medicine, pediatrics, obstetrics and gynecology, psychiatry, and surgery – and a two-week rotation in neurology.
“They get a whole expansive view of the practice of medicine and how the system of healthcare works,” Dr. Sullivan says. “This is the year when students assume the role of a physician, under the supervision of a licensed faculty member, and take histories, perform physical exams, complete notes for attestation in the electronic health record, formulate differential diagnosis, write orders, and perform routine procedures.”
The third and final phase of the program is when students focus on career exploration, scholarship activity, and advanced electives. This is when “they really decide what they want to practice,” Sullivan says, and they focus the majority of their fourth year on advanced rotations. This gives the students an opportunity to further explore their preferred specialties before they have to begin applying to residency programs.
Community-Connected Medical Education
Serving the community is the school of medicine’s main mission, and the community is woven into every phase of the MD program – which Sullivan says is the program’s “most distinctive element.”
Students begin to immerse themselves within the Nevada community through the initial population health course and longitudinal Nevada community service courses throughout the first phase of the program. They become more familiar with the people who reside in the community and learn about the common experiences, ailments, and environments. Students are also assigned to certain districts in Southern Nevada to participate in community service and service learning – which includes learning about community-identified concerns such as transportation and access to medical care.
“They get an all-inclusive look at the patients that they may treat in their clinical studies or beyond,” Sullivan says.
During the third phase, students have to complete the Nevada Community Medicine course and a capstone experience. Sullivan says, “They not only dig a little bit deeper into public health initiatives within the state of Nevada, but they complete public health courses that focus on improving the health of communities and populations, particularly the prevention of disease.”
The MD program is constantly being evaluated through the school’s continuous improvement (CI) process, which ensures that the program remains in a state of perpetual improvement and never wavers from the school of medicine’s mission of providing high-quality innovative education, research, and optimal clinical care to the community.