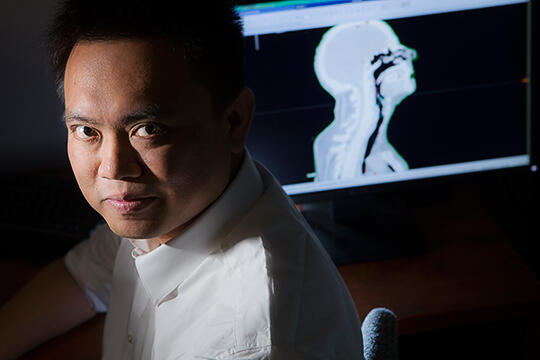
Yu Kuang, an assistant professor in the School of Allied Health Sciences, is focused on the early detection of cancer and image-guided cancer treatment. His recent work explores whether testing for genetic markers associated with tumors, coupled with new approaches to quantitative magnetic resource imaging (MRI) analysis, might lead to more effective treatments for sarcomas, malignant tumors that form in bone, cartilage, fat, muscle, or vascular tissue.
Patients diagnosed with sarcoma usually undergo what health care providers call "neoadjuvant" therapy -- typically chemotherapy -- to shrink their tumors before surgery. Reducing tumor size prior to operating, oncologists have found, not only makes surgery more effective but also enhances patients' long-term survival rates.
A drawback of this approach is that determining whether neoadjuvant therapy has done its job can only happen via tumor-tissue analysis following surgery. This means that patients don't learn if they've benefitted until after leaving the operating room, an unfortunate reality that ensures some patients will endure the toxic effects of chemotherapy without any therapeutic advantage. For these patients, the harm in superfluous chemo is not just in the unnecessary discomfort it inflicts. Precious time has been wasted -- time that could have been spent on potentially life-saving treatment alternatives.
Kuang has teamed up with the Children's Specialty Center of Nevada and Nevada Imaging Centers to develop an earlier, non-invasive method for predicting success or failure of neoadjuvant chemotherapy. His method involves combining an analysis of tumor markers in mitochondrial DNA from blood draws and diffusion MRI data. The goal, Kuang says, is to identify the early changes of genetic biomarker levels in the blood and the imaging features in the MRI scan that can help clinicians more effectively ascertain how well sarcomas have responded to pre-operative chemotherapy.
By determining patients' response to the treatment early in the course of chemotherapy, Kuang's team expects this research will ultimately enable oncologists to optimize treatment protocols for individual patients, improving quality of life and enhancing disease-free survival for patients with sarcoma.
If successful, Kuang's next step will likely involve multi-institutional clinical trials. These will seek to determine how this combined biological- and imaging-biomarker method might be used to guide future chemotherapy treatments.
Kuang is also actively involved in multi-institutional collaborative work related to prostate cancer. Earlier this year, he teamed up with Sandi A. Kwee, a physician and associate professor at the John A. Burns School of Medicine at the University of Hawaii, to develop a positron emission tomography (PET) image guided prostate cancer radiation therapy method. PET scan is an imaging test that helps reveal how patients' tissues and organs are functioning via a radioactive drug (radiotracer). In this collaboration, the radiotracer Kuang and Kwee are using is a new U.S. Food and Drug Administration-approved investigational drug that could allow for better targeting of radiation treatments used against intermediate- and high-risk prostate cancer.
The collaborative relationship is expected to lead to a multicenter clinical trial initiative between UNLV and University of Hawaii, a trial that could bring this potentially game-changing approach to prostate cancer patients in Southern Nevada.